Painkiller addiction were never meant to become the villain. They were designed to soothe, to soften suffering, to give the body a breather from chaos. Yet somewhere between relief and reliance, millions find themselves quietly slipping into painkiller addiction not out of recklessness, but out of survival. The truth is, no one wakes up wanting to depend on a pill. Addiction grows slowly, subtly, disguised as healing until it becomes a shadow that refuses to step aside.
Stopping painkiller addiction isn’t about shame. It’s about reclaiming the life the pain tried to take from you.
When Relief Turns Into Reliance
Painkiller addiction symptoms often start small. A body that once needed a pill occasionally now seems to “need” it to get through the day. A prescription meant for a short period becomes a routine that feels impossible to break. You begin noticing the shifts ,not sleeping without it, feeling irritable between doses, fearing the next wave of pain more than the drug itself.
The cruel irony is that the same medication painkiller addiction that offered comfort eventually rewires the nervous system. The brain grows dependent on the chemical quiet, and everyday discomfort feels unbearable in comparison. This is not weakness; it is neurobiology.
Understanding that difference is the beginning of recovery.
Recognizing Painkiller Addiction Signs Early
Painkiller addiction signs are often emotional before they’re physical. You may find yourself planning your day around your next pill, feeling panic at the thought of running out, or inventing reasons to justify just one more dose. The body plays along, too , nausea, sweating, anxiety, restless legs, and mood swings.
And then come the deeper painkiller addiction effects: slowed breathing, constipation, memory fog, hormonal imbalances, and a kind of emotional numbing that makes you feel like you’re moving through someone else’s body. The longer dependence lingers, the more the brain forgets how to regulate itself without chemical assistance.
But the brain is adaptable beautifully, stubbornly adaptable. That’s the hope.
Painkiller Addiction Withdrawal: The Hardest Door to Walk Through
Painkiller addiction withdrawal is uncomfortable, but it is not impossible, and more importantly, it is temporary. Your body is relearning how to feel again. People often describe withdrawal as waves: chills, muscle aches, insomnia, mood swings, cravings that come and fade.
This phase can be dangerous if unsupervised, which is why medical detox exists. No one should have to white-knuckle their way out of a neurochemical storm alone.
Detox isn’t weakness,it’s strategy.
How Painkiller Addiction Treatment Actually Works
Stopping painkiller addiction isn’t about simply “quitting.” If it were that easy, no one would struggle. Effective painkiller addiction treatment is layered, intentional, and tailored to your life. Think of it as rehabilitating your nervous system ,teaching it how to regulate pain, emotion, and stress without leaning on opioids.
Recovery usually involves:
- Medical detox to safely manage withdrawal
- Therapeutic support to understand the emotional roots of dependence
- Medication-assisted treatment (like buprenorphine or methadone) when appropriate
- Psychotherapy, especially trauma-informed approaches
- Lifestyle restructuring, from sleep hygiene to diet to physical movement
- Relapse-prevention planning, because accountability protects progress
Treatment isn’t about judgement ,it’s about rebuilding agency.
Emotional Healing in Painkiller Addiction Recovery
Painkiller addiction rarely exists without a story underneath it. Sometimes it begins with injury, surgery, or chronic illness. Sometimes it begins with emotional pain disguised as physical pain. Trauma and opioids often intersect ,one numbs the body, the other numbs the mind.
Healing requires both layers.
Addressing the emotional landscape ,grief, loneliness, burnout, childhood wounds ,is what ensures recovery lasts. People don’t relapse because they’re weak; they relapse because the original pain was never addressed. Therapy reconnects the dots so you don’t have to carry that pain in silence anymore.
Can Painkiller Addiction Lead to Other Health Issues? Absolutely.
Long-term misuse can affect breath, heart rate, digestion, hormones, sleep, cognition, and emotional stability. But the most destructive complication is silence ,the shame that convinces people they’re battling this alone.
Breaking the silence is not vulnerability. It is a strength.
And yes, painkiller addiction can escalate, sometimes into stronger opioids, sometimes into mental health struggles,but intervention at any stage can reverse the damage. Bodies recover. Brains rewire. Lives come back.
Is Painkiller Addiction Recovery Possible?
One of the most hopeful truths about painkiller addiction is that recovery isn’t rare; it’s common. People come back from this every single day. The nervous system is resilient. The body heals. Clarity returns. Identity returns. Future returns.
Painkiller addiction recovery isn’t a miracle; it’s a process. And that process starts with deciding you don’t want to live half-alive anymore.
If you are reading this, that decision might already be forming.
FAQs
-
What is painkiller addiction?
It’s a physical and emotional dependence on opioid or opioid-like medications, where the body and brain begin to rely on the drug for regulation, comfort, and functioning.
-
What treatments are available for painkiller addiction?
Medical detox, therapy, medication-assisted treatment, support groups, and long-term relapse-prevention strategies form the backbone of effective painkiller addiction treatment.
-
Can painkiller addiction lead to other health issues?
Yes. Respiratory problems, heart issues, digestive dysfunction, hormonal imbalance, sleep disorders, and mental health complications can all arise from prolonged misuse.
-
Is it possible to recover from painkiller addiction?
Absolutely. With treatment, support, and consistent care, recovery is not only possible, it’s common. The brain can heal, and so can you.
How can Samarpan help?
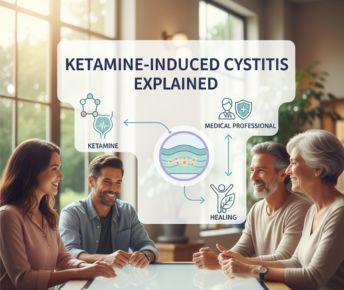
At Samarpan Recovery Centre, Asia’s most trusted drug rehabilitation and mental health facility, we understand that painkiller addiction can develop silently—often beginning with legitimate medical prescriptions and progressing into dependency. Many individuals struggle to recognise the early painkiller addiction signs, mistaking increased tolerance or cravings for normal physical adaptation.
Over time, the side effects of painkiller addiction—including mood changes, fatigue, poor concentration, and withdrawal pain—begin to take a toll on both mental and physical health. Our specialised programs address every stage of recovery, from managing painkiller addiction withdrawal safely under medical supervision to providing long-term painkiller addiction treatment through evidence-based therapies like CBT, DBT, and trauma-focused counselling.
At Samarpan, we don’t just treat symptoms—we uncover the root causes behind painkiller addiction effects, whether emotional pain, trauma, or untreated anxiety and depression. Our multidisciplinary team creates personalised care plans that include medical detox, psychotherapy, and holistic wellness interventions to restore balance and resilience.
With structured relapse prevention strategies and compassionate support, we guide individuals on how to stop painkiller addiction safely and sustainably. Samarpan’s world-class infrastructure, dedicated clinicians, and trauma-informed environment make it a leading destination for lasting healing and recovery.





















 Yes, many offer serene environments and solid therapeutic frameworks. However, quality varies, so it’s essential to research accreditation, staff credentials, and therapeutic depth.
Yes, many offer serene environments and solid therapeutic frameworks. However, quality varies, so it’s essential to research accreditation, staff credentials, and therapeutic depth.




